what is remote patient monitoring
Enhancing Care from Afar: Understanding What Is Remote Patient Monitoring
In an era where technology is revolutionizing all aspects of life, healthcare is no exception. Remote patient monitoring (RPM) is emerging as a trailblazer, transforming how patients interact with their healthcare providers and manage their own health. But what is remote patient monitoring exactly, and how does it contribute to improving patient outcomes while making healthcare delivery more efficient?
Key Takeaways
- Remote Patient Monitoring (RPM) utilizes devices like blood pressure monitors and glucose meters to help healthcare providers monitor and manage patients’ health conditions remotely, improving chronic disease outcomes and reducing the need for hospital readmissions.
- RPM offers significant advantages by enhancing patient access to care, particularly for those in remote or underserved areas, improving patient engagement and personalized care, and generating cost savings and efficiencies within healthcare systems.
- RPM implementation requires careful planning, including identifying patient needs, selecting the right technology, and educating both staff and patients. Regulatory and reimbursement considerations are also critical, with specific billing codes and best practices to be followed for compliance.
Defining Remote Patient Monitoring (RPM)

Remote Patient Monitoring, abbreviated as RPM, is a method of healthcare delivery. It enables providers to keep track of patients outside the usual clinic environment through remote patient monitoring programs. This method proves particularly beneficial for managing chronic and acute conditions when direct, in-person care is not an option. Remote physiologic monitoring services include the use of RPM devices, ranging from:
- blood pressure monitors
- glucose meters
- heart rate monitors
- pulse oximeters
enable healthcare providers to observe, record, and assess their patients’ health conditions, even from afar. This remote care approach is proving effective in managing a range of chronic conditions, including heart disease, diabetes, and chronic obstructive pulmonary disease (COPD).
RPM devices serve as more than mere health gadgets. They function as lifelines, enabling healthcare providers to stay attuned to the health of their patients, particularly those grappling with chronic conditions. They provide a constant stream of real-time health data that can be critical for disease control, making them an essential part of modern healthcare systems.
The Role of RPM in Healthcare
In the sphere of patient care, RPM is emerging as a revolutionary tool. It enables healthcare providers to access real-time health data, empowering them to make proactive clinical decisions based on the most current information available. Beyond just data collection, RPM breaks barriers to healthcare access. It eliminates the need for patient transportation, allowing patients to receive care right at their homes. This is especially beneficial for patients with conditions like high blood pressure, where regular monitoring is essential.
Furthermore, RPM effectively manages hospital space by:
- Allowing the monitoring and care of less critically ill patients outside the hospital environment
- Reducing hospital crowding
- Preserving space for those with more critical needs.
Key Components of RPM
An RPM system is much more than just the monitoring devices. It’s a complex arrangement of interconnected components that work together to ensure seamless monitoring and data transmission. The essential components of an RPM system are the devices, the data transmission method, and the healthcare provider’s role in monitoring and management.
RPM devices are generally designed with simplicity in mind, thus reducing the necessity for continual technical support and lowering the possibility of patient dissatisfaction. The data collected by these devices is transmitted over a cellular network or via Bluetooth technology, depending on the device and the healthcare provider’s preference. When selecting between these technologies, it’s essential to consider factors such as service coverage, connectivity limitations, and the benefits and limitations of each technology solution.
Advantages of Remote Patient Monitoring
As RPM’s role in healthcare broadens, its benefits are becoming more and more apparent. RPM offers a streamlined and impactful method for healthcare professionals to:
- closely monitor chronic health conditions in patients without necessitating in-person appointments
- improve patient involvement and adherence to treatment regimens
- extend the reach of physicians, facilitating care provision without mandating patient transportation.
RPM offers patients personalized attention from healthcare providers, improved understanding and management of their conditions, and the convenience of accessing care from their homes or remote locations, all of which result in significant advantages. By enabling continuous real-time condition monitoring and management, RPM enhances patient outcomes by expediting access to healthcare providers, lowering hospital readmission rates, and offering assistance to socially isolated patients.
Improved Patient Outcomes
RPM aids in enhancing patient outcomes by:
- Permitting ongoing monitoring and management of patients’ health conditions
- Providing patients with valuable insights into their conditions
- Encouraging proactive healthcare
- Improving specific chronic disease outcomes
- Enabling real-time access to data
- Fostering better communication between healthcare providers and patients
RPM ultimately leads to improved outcomes and increased patient engagement.
RPM has been shown to enhance patient outcomes in areas such as chronic disease management, post-operative care, and remote monitoring of COVID-19 patients, leading to decreased necessity for hospital visits. Medical conditions such as cardiac diseases, diabetes, and asthma have exhibited improved outcomes as a result of RPM, which enables continuous monitoring of vital signs essential for managing these conditions.
Enhanced Access to Care
RPM is instrumental in bridging the divide between patients and healthcare providers. It plays a significant role in:
- improving access to healthcare services, especially for patients residing in remote or underserved areas
- making geographical boundaries less of a barrier
- making quality healthcare more accessible
It’s not just patients in remote areas who stand to benefit. RPM can also play a significant role in providing care for patients who may have difficulty leaving their homes due to physical limitations or health risks. This enhanced access to care, coupled with the convenience of receiving care at home, can significantly improve the patient experience and contribute to better health outcomes.
Cost Savings and Efficiency
Finally, the financial consequences of RPM must not be disregarded. RPM contributes to reducing healthcare costs significantly by:
- Lowering chronic illness management expenses
- Preventing hospital readmissions
- Eliminating unnecessary office visits
- Enhancing patient adherence and satisfaction
These factors ultimately lead to a reduction in both individual and overall healthcare costs.
Moreover, RPM contributes to the efficiency of healthcare delivery by:
- Facilitating continuous transmission of crucial health data
- Promoting clinical efficiency
- Decreasing emergency room visits and hospital stays
- Improving physician productivity
- Streamlining processes through the automation of health data recordings
- Ultimately freeing up resources and time for healthcare professionals.
Common Remote Patient Monitoring Devices
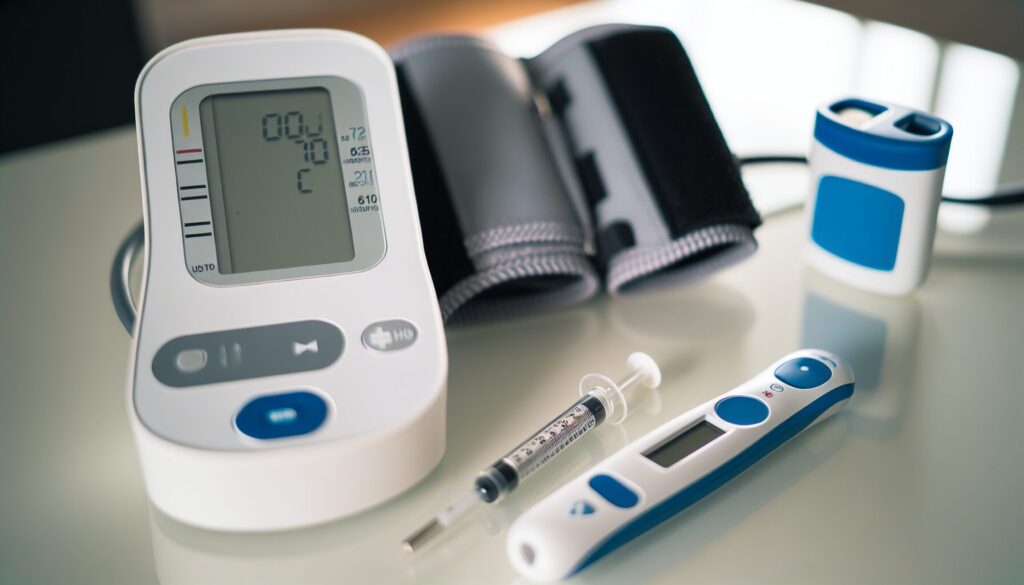
Having clearly understood what RPM entails and its advantages, it’s time to explore the devices that enable it. Some of the most widely used RPM devices include:
- Weight scales
- Blood pressure monitors
- Pulse oximeters
- Blood glucose meters
These devices provide crucial data that helps healthcare providers monitor patients and manage their health conditions.
Whether it’s a pulse oximeter helping monitor patients with chronic heart or lung conditions, including COPD, CHF, asthma, and pneumonia, or a blood pressure monitor playing a crucial role in RPM programs, especially for patients with hypertension, these devices provide a lifeline for patients suffering from chronic conditions. Let’s examine some of these devices in greater detail.
Blood Pressure Monitors
Monitoring blood pressure is essential for patients with hypertension and other conditions to effectively manage their health conditions. RPM devices, such as blood pressure monitors, provide a convenient and accurate way for patients to monitor their blood pressure at home, removing the need for frequent in-person visits to the doctor’s office.
The American Heart Association advocates for the remote monitoring of vital signs for patients with hypertension, citing research studies that demonstrate the benefits of RPM. Thus, blood pressure monitors have become an important tool in the arsenal of RPM devices.
Glucose Meters
For patients with diabetes, monitoring blood glucose levels is crucial. RPM devices like glucose meters can play a significant role in managing diabetes by providing real-time monitoring of glucose levels.
Moreover, RPM offers diabetes patients continuous monitoring, allowing healthcare providers to make timely adjustments in medication regimens and provide recommendations. It also benefits endocrinologists by providing regular blood sugar readings and has been shown to effectively control HbA1c levels in people with type 2 diabetes.
Wearable Devices

In the world of RPM devices, wearable devices hold a special place. From activity trackers like Fitbit or Apple Watch to continuous monitoring wearables in the form of stickers or patches, these devices are making RPM more accessible and convenient.
These wearable devices collect real-time medical data from the wearer and transmit it to the internet for further analysis or feedback from healthcare providers. The data can be transmitted through the integration of hardware, software, and mobile applications, allowing for remote monitoring and timely interventions.
Implementing a Successful Remote Patient Monitoring Program
Implementing an RPM program involves more than merely distributing devices to patients. It involves identifying a specific patient need, selecting appropriate devices, and training the staff on how to use and manage these devices. Understanding the needs of your patients and selecting the right technology are crucial steps in implementing a successful RPM program.
However, the task doesn’t end at that point. Training staff and educating patients is equally important to ensure the effective operation of the program. From dealing with data flow to patient education, each step requires careful planning and execution.
Identifying Patient Needs
Identifying the specific needs of your patients is the first step in setting up an RPM program. By understanding what patients need, healthcare providers can tailor the RPM program to meet these needs, making it more effective and successful.
Patient needs can vary widely, influenced by factors such as:
- age
- health condition
- lifestyle
- education
- income level
- location
By understanding these factors, healthcare providers can personalize RPM interventions, enhancing the quality of care for each patient and enabling providers to customize monitoring and management based on the patient’s unique circumstances.
Selecting the Right Technology
Selecting the right technology is another crucial step in implementing an RPM program. Factors to consider when choosing RPM devices include:
- Technical feasibility
- Patient suitability
- Integration with electronic medical records (EMR)
- Data actionability
- Connectivity
When it comes to data transmission, the devices can transmit data over a cellular network or via Bluetooth technology, depending on the device and the healthcare provider’s preference. But it’s important to consider factors such as service coverage, connectivity limitations, and the benefits and limitations of each technology solution when making this decision.
Training Staff and Educating Patients
Once the needs have been identified and the right technology has been selected, the next step is training staff and educating patients. Staff need to be trained on how to manage data flow and ensure effective program operation.
For patients, education about RPM is crucial. It’s important to define the concept and understanding of how it works, alongside implementing a platform that helps healthcare organizations stay connected to their patients. This education can help improve patient engagement and treatment adherence, leading to better health outcomes.
Regulatory and Reimbursement Considerations
The introduction of any new healthcare service brings along a slew of regulatory and reimbursement considerations. RPM is no exception. Understanding the regulatory landscape is crucial for healthcare providers implementing RPM services. Key considerations include Medicare and Medicaid services, private payer policies, and compliance and billing best practices.
As with any healthcare service, ensuring compliance with RPM billing requirements is of utmost importance to avoid potential issues such as audits and non-payment. Understanding and correctly applying the four specific codes for billing RPM services is crucial. These codes are:
- 99453
- 99454
- 99457
- 99458
Medicare and Medicaid Services
The role of the Centers for Medicare & Medicaid Services (CMS) in reimbursing RPM services is to:
- Establish guidelines and coding requirements for reimbursement
- Determine whether the services are medically reasonable and necessary
- Ensure that they are not duplicative of other services.
Understanding the CMS guidelines pertaining to the utilization of CPT codes for RPM services is crucial for ensuring proper billing. These guidelines encompass the following CPT codes for remote patient monitoring:
- 99091: covers device setup and patient onboarding
- 99453: covers remote monitoring of physiologic parameters
- 99454: covers device supply with daily recording or programmed alert transmission
- 99457: covers remote physiologic monitoring treatment management services
- 99458: covers remote physiologic monitoring treatment management services, additional time
These codes cover a range of remote patient monitoring aspects, including device setup, onboarding, and ongoing monitoring.
Private Payer Policies
Beyond Medicare and Medicaid, many commercial payers are also including RPM in their telehealth coverage policies. Private insurance companies often align their RPM coverage with the standards set by Medicare, easing the process for providers already familiar with CMS guidelines.
However, coverage and reimbursement policies can vary widely among private payers. It’s important for providers to understand the specific policies of each payer they contract with to ensure they are maximizing reimbursement while remaining compliant with all guidelines.
Compliance and Billing Best Practices
Billing for RPM services can be complex, but by adhering to best practices and complying with regulations, providers can ensure they are maximizing reimbursement while avoiding potential issues such as audits and non-payment. Key to this is understanding and correctly applying the four specific codes for billing RPM services:
- 99453
- 99454
- 99457
- 99458
In addition, providers should:
- Ensure meticulous documentation
- Conduct internal audits
- Comprehend their data
- Be aware of denial rates and take steps to reduce them
- Implement correct coding and billing
Having a clear understanding of potential audit risks and taking steps to minimize these risks can help ensure a successful RPM program.
The Future of Remote Patient Monitoring
Looking forward, it’s evident that RPM will play a significant part. With advancements in technology and expanded research into new diseases that can be remotely managed, RPM is expected to experience substantial growth as a crucial component of healthcare.
RPM has the potential to:
- Improve patient safety by preventing adverse events
- Enhance the patient experience through continuous and proactive health management
- Lead to significant cost savings, making healthcare more accessible and affordable for all.
Technological Innovations
RPM is fundamentally driven by technology, and with technological advancements, RPM’s capabilities will also evolve. Artificial intelligence is being integrated into RPM through personalized support, reminders, and insights for medication adherence, and alerting healthcare teams when vital signs are outside of normal ranges.
Machine learning, another emerging technology, is enhancing RPM by:
- Analyzing extensive patient data to recognize patterns
- Making health predictions
- Aiding in early detection
- Personalized treatments
- Proactive measures
- Patient self-management
- Improving clinical priorities and efficiency.
Expanding Use Cases
As RPM keeps evolving, its applications will also expand. Currently, RPM is used primarily for managing chronic conditions, but there is potential for it to be applied in new areas of healthcare. For instance, RPM contributes to improving post-surgical care by facilitating home monitoring for patients, thereby enhancing care coordination and post-surgery management.
Similarly, several studies provide evidence supporting the efficacy of RPM in mental health care, showing that RPM programs:
- Improve the connection and communication between healthcare staff and patients
- Lead to proactive support for symptomatic patients
- Enable the delivery of patient-centric care.
Integration with Other Healthcare Services
Integrating RPM with other healthcare services marks a crucial stride towards establishing a comprehensive and efficient healthcare system. For instance, RPM integration with virtual-first health plans involves enabling RPM-enabled members to track and report their biometrics, such as blood pressure and glucose levels, to their virtual primary care providers.
Moreover, the integration of RPM with hospital-at-home programs provides numerous advantages, including:
- Enhanced ongoing care and monitoring
- Early intervention to mitigate hospitalization
- Continuous monitoring of biometrics
- Reassurance of oversight
- Recording and transmission of patient data to care teams, fostering improved communication and coordination of care.
Summary
As we’ve seen, RPM holds great promise as a revolutionary tool in healthcare. By enabling continuous patient monitoring, enhancing access to care, reducing healthcare costs, and offering a range of beneficial devices, RPM is poised to transform the healthcare landscape. With advancements in technology and expanding use cases, the future of RPM looks bright. As we move forward, it’s clear that RPM will play a crucial role in shaping the future of healthcare, making it more efficient, accessible, and patient-centric.
Frequently Asked Questions
What does a remote patient monitoring do?
Remote patient monitoring allows patients to use mobile medical devices to gather health data and send it to healthcare professionals, historically used for chronic conditions like cardiac diseases and diabetes.
What is the difference between telehealth and remote patient monitoring?
The main difference between telehealth and remote patient monitoring is that telehealth encompasses a broader field, including technologies for engaging with patients remotely, while remote patient monitoring is just one application of telehealth.
How is remote monitoring done?
Remote monitoring is conducted using digital medical devices, allowing healthcare providers to keep track of patients outside the traditional care setting.
What is Remote Patient Monitoring (RPM)?
Remote Patient Monitoring (RPM) is a method that allows healthcare providers to monitor patients with chronic or acute conditions between clinic visits or when in-person care is not feasible. It helps in managing patient care effectively.
What are some common RPM devices?
Some common RPM devices include weight scales, blood pressure monitors, pulse oximeters, and blood glucose meters. These devices help track various health indicators and support remote patient monitoring.